A- Cervix is the lowermost end of the uterus, which connects the uterus with the vagina. When the cancer starts in the cervix, it is known as cervical cancer.
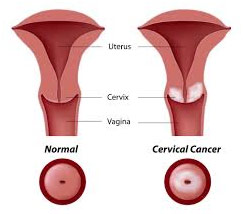
1. What is cervical cancer?
2. How common is it in India?
A- Cervical cancer ranks as the second cause of female cancer in India. Every year 1,27,356 women are diagnosed with the cervical cancer and about 79,906 women die from the disease as per the statistics of year 2022. The peak age for the cervical cancer incidence is 50-59 years.
3. What causes cervical cancer?
A- Persistant Human Pàpilloma virus infection is required for causing Cervical Cancer and it is transmitted by skin to skin contact commonly during unprotected sexual contact with an infected person
4. How common is HPV infection?
A- Each year HPV is related with 1,32,000 new cases of cervical cancer and 79,000 deaths due to cervical cancer. In India 87.8 to 96.67 percent of women with cervical cancer are infected with HPV. HPV infection is most prevalent between the ages of 26 and 35.
Reference:- NICPR ICMR, Cancer Statistics – India Against Cancer [ Internet ] 2022 356- india-fact-sheet.pdf
https://gco.iarc.fr/tomorrow/graphic-isotype?type
5. What are the risk factors to get cervical cancer?
A- Several risk factors for acquiring the HPV infection are:
- Early age at marriage
- Multiple sexual partners
- Multiple pregnancies
- Poor genital hygiene
- Malnutrition
6. What are the early signs of the cervical cancer?
A- Watch out for the following warning signs:
- Bleeding between periods
- Bleeding during or after sex
- Any unpleasant vaginal discharge
- Bleeding after menopause
- Discomfort or pain during sex
7. What screening techniques are available for cervical cancer?
- Pap smear
- VIA (visual inspection with acetic acid)
- VILI (visual inspection with lugol’s iodine)
- HPV DNA test
All of these examinations are basic and take approximately five minutes. They are typically painless, however some women may experience some discomfort.
8. How are these tests performed?
A- These tests essentially check the cervix for abnormal cells. This is accomplished by a variety of means, including the ones listed below:
- Taking the sample of the abnormal cells at the cervix with a brush and examining it under the microscope (Pap smear).
- Staining the cervix with the dilute acetic acid (vinegar) and looking for distinct white areas which are suggestive of abnormal cells.
- Taking the sample from the cervix to look for the presence of the human papilloma virus (HPV) which is responsible for causing cervical cancer in most of the cases.
9. Where are these tests carried out?
A- They can be easily performed by the doctors at all the district level hospitals. It requires very minimal time to do the test.
10. Why is cervical cancer screening important?
A- According to the studies, HPV infection might take about a decade to progress to the invasive cancer, therefore giving enough time for the preventive methods. About 5000-6000 lives are saved every year by the simple screening methods.
| STAGE OF CANCER | 5 YEAR SURVIVAL RATE |
| 0 | 93% |
| 1A | 93% |
| 1B | 80% |
| 2A | 63% |
| 2B | 58% |
| 3A | 35% |
| 3B | 32% |
| 4A | 16% |
| 4B | 15% |
The term 5 year survival rate is commonly used to indicate the outlook of cervical cancer, i.e. the percentage of persons who will live for at least 5 years after their cancer is detected. The rates in Table 2 were published in the 7th edition of the AJCC staging manual in 2010 and provide the most recent data on the survival rate.
As seen in the table, this cancer has a very excellent prognosis if detected early, but a terrible prognosis if detected late. Herein lies the significance of screening; if done on time, it can save a lot of headaches.
11. How can cervical cancer be prevented?
A- It can be prevented using 2 strategies :
- Primary Prevention by vaccination against HPV.
There are 2 types of vaccine available: Quadrivalent n Nonavalent .
Quadrivalent vaccines available are Gardasil & Cervavac.
Ideal age of vaccination is 9 to 14 years where 2 doses are given at 0 & 6 months interval & after 15th birthday till 45 years in females 3 doses are recommended… 0, 2, 6 months
In males 9 to 14 years 2 doses & 15 to 26 years 3 doses are recommended.
As per the SAGE, WHO it has been found that single dose shows comparable efficacy to two or three dose schedule & so it is recommended to give single dose from 9 to 20 years n 2 doses from 21 years onwards. - Secondary prevention is by getting your self screened on regular basis or at least at the age of 35 years n 45 years.
Follow up with the Doctor if screening test reports are not normal
Avoid the high risk behaviour.