A- Cervix is the lowermost end of the uterus, which connects the uterus with the vagina. When the cancer starts in the cervix, it is known as cervical cancer.
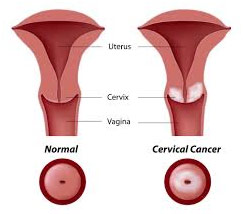
1. What is cervical cancer?
2. How common is it in India?
A- Cervical cancer ranks as the second cause of female cancer in India. Every year 122,844 women are diagnosed with the cervical cancer and about 67,477 women die from the disease. The peak age for the cervical cancer incidence is 55-59 years.
3. What causes cervical cancer?
A- Human papillomavirus infection is a required but not sufficient cause of cervical cancer, which is transmitted by close skin-to-skin contact, such as during unprotected sexual contact with an infected person.
4. How common is HPV infection?
A- Each year, HPV is related with 50,000 new instances of cervical cancer and 250,000 deaths due to cervical cancer. In India, between 87.8 to 96.67 percent of women with cervical cancer are infected with HPV. HPV infection is most prevalent between the ages of 26 and 35.
5. What are the risk factors to get cervical cancer?
A- Several risk factors for acquiring the HPV infection are:
- Early age at marriage
- Multiple sexual partners
- Multiple pregnancies
- Poor genital hygiene
- Malnutrition
6. What are the early signs of the cervical cancer?
A- Watch out for the following warning signs:
- Bleeding between periods
- Bleeding during or after sex
- Any unpleasant vaginal discharge
- Bleeding after menopause
- Discomfort or pain during sex
7. What screening techniques are available for cervical cancer?
- Pap smear
- VIA (visual inspection with acetic acid)
- VILI (visual inspection with lugol’s iodine)
- HPV DNA test
All of these examinations are basic and take approximately five minutes. They are typically painless, however some women may experience some discomfort.
8. How are these tests performed?
A- These tests essentially check the cervix for abnormal cells. This is accomplished by a variety of means, including the ones listed below:
- Taking the sample of the abnormal cells at the cervix with a brush and examining it under the microscope (Pap smear).
- Staining the cervix with the dilute acetic acid (vinegar) and looking for distinct white areas which are suggestive of abnormal cells.
- Taking the sample from the cervix to look for the presence of the human papilloma virus (HPV) which is responsible for causing cervical cancer in most of the cases.
9. Where are these tests carried out?
A- They can be easily performed by the doctors at all the district level hospitals. It requires very minimal time to do the test.
10. Why is cervical cancer screening important?
A- According to the studies, HPV infection might take about a decade to progress to the invasive cancer, therefore giving enough time for the preventive methods. About 5000-6000 lives are saved every year by the simple screening methods.
| STAGE OF CANCER | 5 YEAR SURVIVAL RATE |
| 0 | 93% |
| 1A | 93% |
| 1B | 80% |
| 2A | 63% |
| 2B | 58% |
| 3A | 35% |
| 3B | 32% |
| 4A | 16% |
| 4B | 15% |
The term 5 year survival rate is commonly used to indicate the outlook of cervical cancer, i.e. the percentage of persons who will live for at least 5 years after their cancer is detected. The rates in Table 2 were published in the 7th edition of the AJCC staging manual in 2010 and provide the most recent data on the survival rate.
As seen in the table, this cancer has a very excellent prognosis if detected early, but a terrible prognosis if detected late. Herein lies the significance of screening; if done on time, it can save a lot of headaches.
11. How can cervical cancer be prevented?
A- It can be avoided by using the strategies listed below:
- There are 2 types of the vaccines available to prevent the HPV infection: cervarix and Gardasil. Both are equally effective. The ideal recommended age group for vaccination is 12-26 years; before the first sexual debut. Maximum effectiveness is between 9-13 years. Three injections are given over six months. The vaccine protects against the two types of HPV that cause 7 out of the 10 cervical cancer cases, however, since it doesn’t protect against all types of the HPV, cervical screening is still important.
- Getting yourself screened on the regular basis.
- Follow up with the doctor if the screening tests reports were not normal.
- Avoiding the high risk behaviour.